Imaged parent items
Guide for Nurses
Why pediatric MS is important
- Treating kids is always important
- Many missed opportunities because diagnosis is delayed, yet early treatment is critical
- Studying pediatric MS may increase our understanding of the pathogenesis of the disease and help all patients with MS
Unique Challenges
- The diagnosis of pediatric MS is increasingly being considered
- Wide spread availability of MRI
- Need for early diagnosis & treatment
- Demyelination in the presence of ongoing myelination within the brain raises unique issues
- Rapid diagnosis and treatment is limited by lack of clinical experience
Epidemiology
- 2.5 million people affected world-wide
- 3.5-5%symptoms before 18 years
- (100,000-200,000 world-wide)
- 0.2-0.7% onset before 10 years of age
- MS as young as 2 years is reported but uncommon
Gender Distribution
|
Age |
Female: Male |
Ref |
|---|---|---|
|
< 10 years |
0.6: 1 |
Simone 2002 |
|
10 – 14 years |
2.6:1 |
Simone 2002 |
|
13 years |
3.5:1 |
Boiko 2002 |
|
14 years |
7.5:1 |
Boiko 2002 |
Definitions
- AcuteDisseminated Encephalomyelitis(ADEM)
- Clinical Isolated Syndrome (CIS)
- Neuromyelitis Optica (Devic Syndrome)
- Pediatric Multiple Sclerosis(Pediatric MS)
ADEM
- Acute Demyelinating CNS Disorder
- Usually a one time event
- Typically Affects Children
- Monophasic Course
- Focal or Multi-focal Neurologic S&S
- Multi-focal Demyelinating Lesions (MRI),grey and white matter
- Behavioral/ or Mental Status Changes
- Seizure
- Prodromal Illness (≥70 %)
- Fever, Headache, Nausea/Vomiting/¯Appetite, Lethargy
ADEM: Clinical Characteristics
- Signs & Symptoms evolve over time
- Maximal deficits reached ~ 1-2 weeks
- Resolution
- rapid / or weeks to months
- may / may not be complete
- Repeat MRI®resolution / no new lesions
ADEM: Laboratory Findings
- CSF: mild pleocytosis(↑wbc)
- + ↑ protein
- + OCB (Oligoclonal Bands) / IgG production
- (uncommon -transient)
- MRI: white matter and grey matter lesions
- (bilateral, asymmetric)
- Usually spare periventricular areas
- + Basal ganglia involved
- lesions highly variable size and number
- punctate - large & confluent - tumor-like
- Usually resolve
ADEM FLAIR MRI
At onset

8 wk f/u
ADEM Differential Diagnosis
- Encephalitis / Infection
- Vasculitis
- Leukodystrophy
- Mitochondrial Cytopathies
- Sarcoidosis
- Histiocytic lymphangiomatosis
- Tumors / glioblastoma
- Multiple Sclerosis
INFECTIOUS ILLNESSES
- Measles -20-30% deaths
- Influenza A or B
- Hepatitis A or B,
- Coxsackie virus
- Vaccinia
- winter/spring respiratory viruses
- Herpes virus infections
- (HSV,VZV, HHV6, CMV,EBV)
IMMUNIZATIONS / VACCINATIONS
- Rabies
- Diptheria -Tetnus-Pertussis
- Hepatitis B
- Smallpox
- Vaccines now devoid of neural elements
- Successful immunization programs, virtual eradication of small pox disease
ADEM Evaluation
|
–CSF –Lactate-Pyruvate –Cytology –IgG Index; OCB –R/O CNS infection CSF profile, CSF viral & bacterial cultures PCR- especially for Herpes Simplex Virus Lyme titer Measles Ab |
Blood CBC/diff, Electrolytes, LFTs, ESR T4/TSH, B12, Biotinase ANA, Anticardiolipin Ab, Antiphospholipid Ab, ACE Lupus Anticoagulant VDRL/RPR CADASIL, LHON mutation Mitochondrial gene mutation Lactate-Pyruvate |
ADEM treatment
- Corticosteroids
- Anti-inflammatory and Immunosupressive
- Anecdotal Reports
- Supportive Care
- Symptomatic Treatment
- Therapy targeted to immune-mediated process
- Currently, no treatment trials or proven protocols for ADEM
ADEM- the dilemma
- ADEM considered an acute monophasic illness
- Most clinicians acknowledge ADEM mayrecur
- myriad of terms found in the literature
- biphasic
- multiphasic
- relapsing
- recurrent
- steroid dependent
- Clinicians also acknowledge –
- some children with ADEM may go on to develop MS
Neuromyelitis Optica (Devic's)
- Absolute criteria
- Hx of ON or recurrent ON
- Hx spinal cord symptoms
- Spinal cord lesion(s) extending 3 or more segments
- Normal brain MRI
- CSF shows pleocytosis (>50 leukocytes)
- May show NMO antibodies
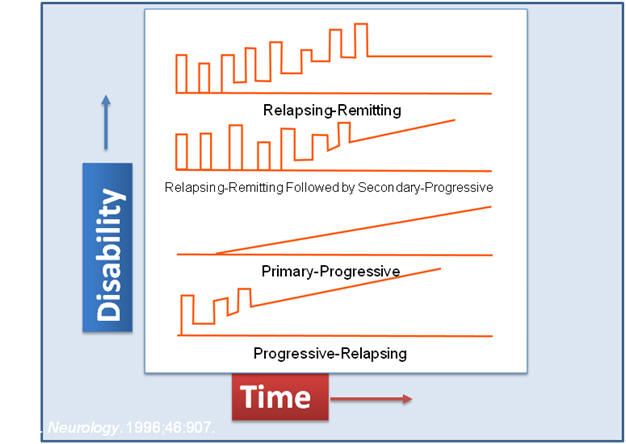
Disease Courses in MS: Types of MS
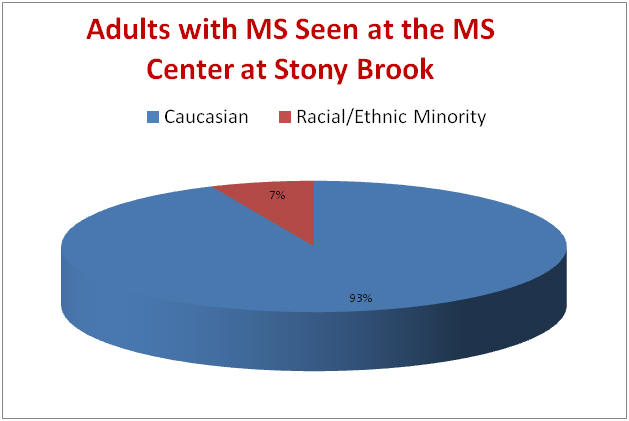
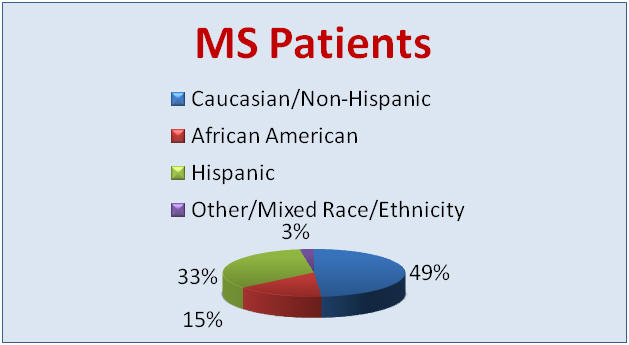
Unusual Demographic Pattern
- Different distribution of ethnic groups among
- adults with MS
- children referred for MS who had other diagnoses
- and children with MS
- More severe in non Caucasians??
Frequency of Pediatric MS
- Data from 149 MS pediatric MS cases from 4 Italian Neurological clinics with 3375 MS patients (Ped MS compared to 923 Adult MS) :
- onset before age 16 (4.4%-7.9%)
- onset before 13 yrs in 1.2%
- onset before 11 yrs in 0.5%
- Ghezzi, Multiple sclerosis, 1997
Why are kids different?
- Exposures
- Immune system “primed”
- Growing pediatric brain…repairs
- Differential in pediatrics
Differences between Adults and Children with MS
- Less common
- More often RR onset
- Overlap in clinical presentation
- Response to disease modifying therapy
- So far seems similar (?)
- Conversion to SP somewhat slower (?)
- Very severe subset (?)
- Demographic pattern may differ?
Differences between Adults and Children with MS
- Average time to recovery shorter
- Kids recover 2-4 weeks faster than adults
- Lower overall disability after attack
- Higher relapse rate
- Shorter time between first and second attack
- Kids may be more likely to have seizures
Pediatric MS Differential Diagnosis
- Structural lesions
- Infectious
- Inflammatory
- Metabolic/Genetic disorders
- Vascular disorders
- Other
Supporting laboratory findings-CSF for MS
- Oligoclonal bands
- IgG index
- Cell count < 50
- Protein usually normal or mildly elevated
- Glucose normal
- All other studies negative
Clinical Features
- Relapsing remitting onset usual course
- ( > 90%)
- Systemic sx occasionally
- Onset may be with sensory, gait, visual or balance problems
- Cognitive problems may be present (33%)
- OCB usually positive
- In some regions of the USA: high number of minorities affected
How do these kids present?
- Optic Neuritis
- Sensory changes
- Motor disturbance
- Ataxia/balance
Presentations in Ped MS
Banwell, Neurology in press
Criteria for Pediatric MS
- Children< 18 years old, includes < 10 years
- Dissemination in space and time (hx and exam)
- No change in mental status typically
- Barkhof MRI criteria
“McDonald” MRI criteria: TIME
- 1st scan < 3 months after clinical event, then repeat 2nd scan 3 months from event
- Gd+ lesion
- if above not met, repeat scan 3 more mos.
- Gd+ lesion or new T2
Clinical Management
- Treatment must involve entire family
- Education, reassurance
- Medication for symptom management
- Urinary dysfunction
- Spasticity
- Depression
- Disease modifying therapy should be given
Experience with Disease Modifying Therapies
- All DMT medications are well tolerated
- Side effects similar to that of adults
- In (< 10 years) on IFN, monitor LFTs at onset
- Clinical impression is that DMT helps reduce relapses and MRI progression
- No data on “best” drug for kids
Experience with DMT
- Some patients require intensive Rx including chemotherapy
- Side effects are few
- Adherence is reasonably high
- Follow-up studies
Experience with Disease Modifying Therapy
- Monotherapy (first line) “ABCR”
- Beta interferon1a (IM or SC and low dose or high dose)
- Avonex, Rebif
- Beta interferon 1b
- Betaseron
- Glatiramer acetate
- Copaxone
- Mitoxantrone
- Beta interferon1a (IM or SC and low dose or high dose)
- Combination Therapy
- DMT with pulse IVIG
- DMT with pulse steroids
- Pulse cytoxan
- One course of high dose cytoxan
Chemotherapy in Pediatric MS
- Novantrone
- Cytoxan
- Imuran
- Rituxumab (Rituxan)
- Natalizumab (Tysabri)
Management of Relapses
- IV Solumedrol: 3 – 5 days (first line) with or without steroid taper
- Second Line:
- Oral steroids moderate or very high doses
- IVIG
- Plasmapheresis
Symptomatic Management
- Attention
- Cognitive rehab, special accommodations
- Fatigue
- Amantadine, modafinil, cooling
- Memory
- Aides, ? Donepezil
- Pain:
- Anticonvulsants, antispasticity agents, anti-inflammatory, physical therapy, exercise
- Depression
- Antidepressants
- Spasticity
- Antispasticity agents, Baclofen pump
- Bladder dysfunction
- Oxybutynin, Self catheterization
- Nutrition
- Rest
- Plan activities
- Heat
- School modifications
- Preferential seating, test modifications, locks, class schedules
Special needs for families with child with MS
- Ped MS patient is isolated
- Families are frightened
- Current support mechanisms are limited
- Special issues relate to school and social interactions
Psychosocial problems
- Challenges sense of self (area of vulnerability in teens)
- Disrupts school
- Lost days
- Emotional changes
- Impaired physical functioning
- Family stress
- Cognitive consequences
Causes of Psychosocial Problems
- Issues specific to MS
- Rare in children
- Physical symptoms (vision,motor, bladder)
- Wax and wane
- Uncertainty of the disease course
- Uncertainty of treatment effect
- Unpleasant treatment modalities
- Injection phobia
- Medication side effects
Consequences
- On the family
- Increased stress and anxiety
- Fear for the future
- Grieving loss of the healthy child
- Variable coping skills
- Financial planning
- Increased stress and anxiety
- On the school experience
- Missed school days
- Lack of awareness by teachers
- Academic declines
- Long range, academic and career planning
Role of health care provider
- Encourage open communication
- Involve family and child with decision making process
- Medication choices to fit child’s lifestyle
- Continuously re-evaluate goals and plans
- Provide reassurance
- Be available to child
- Family
- Emphasize there are others affected, “you are not alone”
- Provide resources, ie on-line secure chat rooms
- Parental telephone support networks
Weekend Retreat
- Unique camp experience for teens and pre-teens with MS
- Kayaking, Ropes Course, Sailing
- Professional recreational therapists
- Nurse practitioner on site; On call MS neurologist
Stony Brook University Hospital
101 Nicolls Road Stony Brook, NY 11794
(631) 444-4000





